Epidural Analgesia
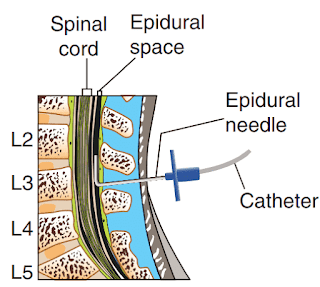
Administration of analgesics into the epidural space is an efficient intervention to manage acute pain. The epidural space is a potential space that contains a network of vessels, nerves, and fat located between the vertebral column and the dura mater, the outermost meninges covering the spinal cord. Analgesics delivered into this space are distributed by (1) diffusion through the dura mater into the cerebrospinal fluid (CSF), where they act directly on the receptors in the dorsal horn of the spinal cord; (2) circulation of blood vessels in the epidural space, from which they are delivered systemically; and/or (3) absorption by fat in the epidural space, creating a depot where the analgesia is slowly released systemically.
Opioids and local anesthetics, separately or in combination, are often used in epidural analgesia. Opioids are delivered close to their site of action (central nervous system) and thus require much smaller doses to achieve the same degree of pain relief. Common opioids administered epidurally include morphine, hydromorphone (Dilaudid), fentanyl, and sufentanil.
ERCP ( Endoscopic Retrograde Cholangiopancreatography): Procedure, Indication, Complications
A patient should be placed in the lateral side-lying or sitting position with the shoulders and hips in alignment and the hips and head flexed during insertion of an epidural catheter. An anesthesia provider places a catheter into the epidural space below the second lumbar vertebra, where the spinal cord ends. However, epidurals may also be placed at the thoracic level of the spinal cord. Catheters intended for temporary or short-term use are not sutured in place and exit from the insertion site on the back. A catheter intended for permanent or long-term use is “tunneled” subcutaneously and exits on the side of the body or on the abdomen. Tunneling reduces the risk for infection and catheter dislodgement. A sterile occlusive dressing covers the catheter exit site and is secured to the patient. An x-ray film is the only way to confirm epidural catheter placement.
The use of epidural opioids requires astute nursing observation and care. The catheter poses a threat to patient safety because of its anatomical location, its potential for migration through the dura, and its proximity to spinal nerves and vessels. Catheter migration into the subarachnoid space can produce dangerously high medication levels. Monitor a patient’s motor and sensory function, including any onset of urinary retention. You should not administer other supplemental opioids or sedatives when patients have been administered an epidural because the combined effect may cause respiratory depression. In many health care agencies, anesthesiologists and nurse anesthetists are the only health care providers who may initiate epidural opioid infusions or administer a medication bolus.
Delegation Considerations
The skill of epidural analgesia administration cannot be delegated to nursing assistive personnel (NAP). The nurse directs the NAP to:
■ Pay particular attention to the insertion site when repositioning or ambulating patients to prevent catheter disruption.
■ Avoid pulling the patient up in bed while he or she is lying flat on the back, which can dislodge the epidural catheter.
■ Immediately report to the nurse any change in level of consciousness.
■ Report any catheter disconnection immediately.
■ Immediately report to the nurse any change in patient status or comfort level.
Abruptio placentae: Causes Risk Factors Diagnostic Study and Treatment
Equipment for Epidural Analgesia
■ Clean gloves
■ Sterile gloves (if removing epidural dressing)
■ Prediluted preservative-free opioid as prescribed by health care provider for use in intravenous (IV) infusion pump (usually prepared by pharmacy)
■ Infusion pump and compatible tubing (Do not use Y-ports for continuous infusion; some infusion pumps have color-coded tubing for intraspinal use.)
■ 20-gauge needleless adapter
■ Filter needle (per agency policy)
■ Syringe
■ Antiseptic swab
■ Sterile gauze pad
■ Tape
■ Label (for injection port)
■ Equipment for vital signs and pulse oximetry
Procedure of Epidural Analgesia
Complete pre-procedure protocol
(A). Verify that catheter is secured to the patient’s skin from the back or front.
(a). Prevents dislodging or migration of catheter.
(B). Assess catheter insertion site for redness, warmth, tenderness, swelling, and drainage. Apply sterile gloves when removing occlusive dressing.
(b) .Catheter sites are at risk for local infections. Purulent drainage is a sign of infection. Clear drainage may indicate CSF leakage from punctured dura. Bloody drainage may indicate that catheter entered blood vessel
(C). Verify health care provider’s order against medication administration record (MAR) for name of medication, dosage, route, infusion method (bolus, continuous, or demand), and lockout settings.
(c). Ensures that right drug is administered to patient. This is the first check for accuracy
(D). For continuous infusion check patency of IV tubing and check infusion pump for proper calibration and operation. Keep IV line patent for 24 hours after epidural analgesia is completed
(d) . Kinked or clamped tubing will interrupt analgesic infusion; may cause clotting at end of IV catheter and require replacement. Patent IV line allows IV access in case medications are needed to counteract adverse reactions.
(E). Prepare analgesia, following “six rights” of medication administration. NOTE: Pharmacy prepares medication for pump. In the case of a bolus injection, draw up prediluted, preservative-free opioid solution through the filter needle into syringe.
(e) .Ensures safe and appropriate medication administration. This is the second check for accuracy.
(F) . Identify patient using two identifiers (e.g., name and birthday or name and account number) according to agency policy. Compare identifiers with information on patient’s MAR or medical record.
(f) .Ensures correct patient. Complies with The Joint Commission requirements for patient safety
(G) . Attach “epidural line” label to the epidural infusion tubing. Be sure that there are no Y-ports for continuous or demand infusions.
(g) .Labeling helps to ensure that analgesic medication is administered into correct line and epidural space. Labeling of high-risk catheters prevents connection with an inappropriate tube or catheter. Using tubing without Y-ports prevents accidental injection or infusion of other medications.
(H). At bedside compare the MAR or computer printout with the name of medication on the drug container.
(h) .This is the third check for accuracy and ensures that the right patient receives the right medication.
(I). Perform hand hygiene, and apply clean gloves.
HEART SOUNDS: S1, S2, S3, S4 and Heart Murmurs
Administer continuous infusion
(A). Attach container of diluted, preservative-free medication to infusion pump tubing, and prime tubing.
(b). Tubing should be filled with solution and free of air bubbles to avoid air embolus.
(B). Insert tubing into infusion pump; then attach distal end of tubing to epidural catheter.
(b). Infusion pumps propel fluid through tubing
(C). Check infusion pump for proper calibration and operation. Many institutions have two nurses check settings.
(c). Ensures patient is receiving proper dose and pain relief.
(D). Tape all connections. Give ordered bolus, or start infusion.
(d). Taping maintains a secure, closed system to help prevent infection. Sometimes a filter is necessary in the tubing.
Administer bolus dose of medication:
(A). Take prepared syringe, and change filter needle to regular 20-gauge needleless adapter.
(b). Prevents infusion of microscopic glass particles and allows medication to be injected.
(B). Clean injection cap of epidural catheter with antiinfective according to agency policy. (Do not use alcohol.)
(b). Cleaning agent prevents introduction of microorganisms into the central nervous system. Alcohol causes pain and is toxic to neural tissue.
(C). Dry injection cap with sterile gauze.
(c). Reduces possible injection of antiseptic
D. Insert needleless adapter of syringe into injection cap. Aspirate.
(d) . Aspiration determines position of catheter. Should aspirate less than 1 mL of clear fluid.
(E). Inject opioid at a rate of 1 mL over 30 seconds.
(e). Slow injection prevents discomfort by lowering the pressure exerted by fluid as it enters the epidural space.
(F). Remove syringe from injection cap. There is no need to flush with saline.
(f) . The catheter is in a space, not a blood vessel; thus flushing with saline is not required.
(G). Dispose of syringe in sharps container.
(g). Prevents possible exposure to blood.
Complete postprocedure protocol
Recording and Reporting
■ Record drug, dose, method (bolus, demand, or continuous), and time given (if injection) or time begun and ended (if demand or continuous) on appropriate medication record. Specify concentration and diluent.
■ With continuous or demand infusion, obtain and record pump readout hourly for first 24 hours after infusion begins and then every 4 hours. Review pump settings and usage together with staff starting the next shift.
■ Record regular periodic assessments of patient’s status in nurses’ notes, in electronic health record (EHR), and/or on appropriate flow sheet, including vital signs, pulse oximetry, intake and output (I&O), sedation level, pain severity score, neurological status, the appearance of the epidural site, presence or absence of adverse reactions to medication, and presence or absence of complications resulting from placement and maintenance of epidural catheter.
■ Report any adverse reactions or complications to the health care provider immediately.
UNEXPECTED OUTCOMES
(A). Patient states pain is still present or has increased. Primary causes are insufficient drug dose or catheter blockage, breakage, or improper position.
: Check all tubing, connections, medication doses, and pump settings.
: Report to health care provider adequacy of medication dose.
(B). Patient is sedated or not easily arousable.
: Stop epidural infusion and elevate patient’s head of bed 30 degrees (unless contraindicated).
: Prepare to administer opioid-reversing agent per health care provider’s order.
: Monitor all vital signs, pulse oximetry, and sedation level continuously until patient is easily aroused
(C). Patient experiences periods of apnea or respirations are less than 8 breaths per minute, shallow, or irregular.
: Instruct patient to take deep breaths.
: Notify health care provider.
: Prepare to administer opioid-reversing agent, such as naloxone (Narcan), per health care provider’s order. (Agency manual may have protocol.)
: Monitor at least every 30 minutes until respirations are 8 breaths or more per minute and of adequate depth for 2 hours.
(D). Patient reports sudden headache. Clear drainage is present on epidural dressing or more than 1 mL of fluid is aspirated from catheter. Possible indication that catheter has migrated into the subarachnoid space.
: Stop infusion.
: Notify health care provider.
(E). Blood is present on epidural dressing or aspirated from the catheter. Probable indication that catheter has punctured a blood vessel
: Stop infusion.
: Notify health care provider
(F). Redness, warmth, tenderness, swelling, or exudate is noted at catheter insertion site. These are signs and symptoms of infection.
:Notify health care provider
(G). Patient experiences minimal urinary output, urinary frequency or urgency, bladder distention, pruritus, or nausea and vomiting.
: Consult with health care provider about reducing the dose of opioids, and discuss treatment for side effects.
Reference Mosby Nursing skills and procedure
Buy the book:



.jpg)



No comments:
Post a Comment
please do not enter any spam link in the comment box